UNE révolution médicale majeure
LE BOOSTER POUR CICATRISER, RÉPARER ET RAJEUNIR
La régérération tissulaire grâce aux PRP (Platelet-Rich Plasma),
PRF (Platelet-Rich fibrin), Bone Morphogenetic Protein (BMP2)
et les cellules souches
LA DENTISTERIE RÉGÉNÉRATIVE
LE BOOSTEuR POUR CICATRISER, RÉPARER, RAJEUNIR les tissus durs et mous
" LA FOLIE EST DE FAIRE TOUJOURS LA MÊME CHOSE ET DE S'ATTENDRE À UN RÉSULTAT DIFFÉRENT "
ALBERT EINSTEIN
Le PRF ou Platelet-Rich Fibrin ou Plasma Riche en Fibrine est apparu quelques années après le PRP.
Ce sont les docteurs Schleicher et Joseph Choukroun (médecin anesthésiste à Nice) qui ont introduit le concentré plaquettaire autologue sans apport d’antiagrégant plaquettaire dans la gestion des douleurs postopératoires.
Le point de départ du Dr Joseph Choukroun a été l’élaboration d’un protocole thérapeutique médical introduisant des concentrés plaquettaires autologues sans apport d’antiagrégant plaquettaire qui puisse être utilisée dans les plaies superficielles nécrosantes.
Ces concentrés plaquettaires autologues activent le processus de fabrication des vaisseaux sanguins, appelé angiogénèse et donc la régénération et la cicatrisation des tissus lésés.
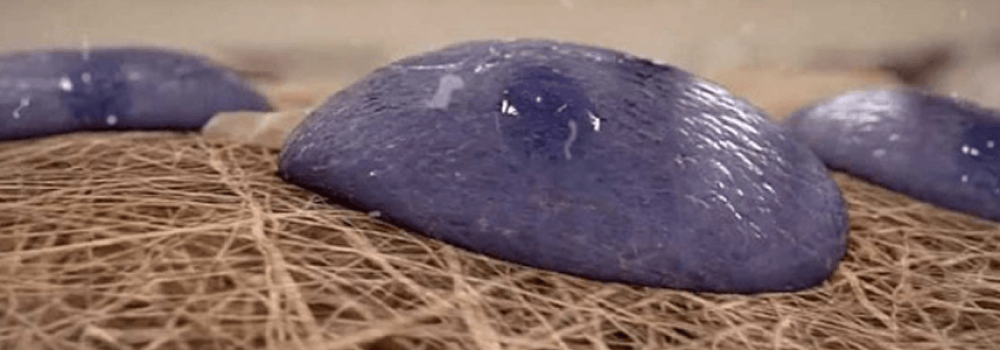
Le PRF ne contient aucun anticoagulant ou antiagrégant plaquettaire, ni aucun autre sous-produit sanguins. Ainsi, il exploite la faculté de la fibrine à réaliser un treillis réticulé qui emprisonne les plaquettes sanguines et les cellules cicatricielles.
Ainsi, le PRF induit plus longtemps dans le temps et d’une façon rémanente, la multiplication et la différentiation des fibroblastes et des ostéoblastes qui participent à la fabrication de nouveaux tissus mous (gencive) et tissus durs (tissus osseux).
Le PRP (également appelé Plasma Riche en Plaquettes) et le PRGF (également appelé Plasma Rich in Growth Factor) sont les premières générations de concentrés sanguins plaquettaires autologues contenant des facteurs de croissance.
Le Professeur Arun K. Garg a décrit et rapporté les protocoles de récupération du PRP. Il a réalisé le grand potentiel thérapeutique dans les techniques chirurgicales que présente ce concentré plaquettaire, extrait par une simple prise de sang sur le patient.
Les applications aux USA dans les domaines de la chirurgie orale, en particulier lors de la pose d’implant dentaire et de chirurgies préimplantaires comme les comblements osseux et les élévations de sinus (sinus lift).
Le PRP a été développé avant le PRGF ou Plasma Rich in Growth Factor ou Pasma Rich en Facteur de Croissance.
Celui-ci a été développé par le docteur Anuita en 1999. Ces deux concentrés sanguins plaquettaires autologues comportent des sous-produits sanguins d’origine animal : des anticoagulants ou antiagrégants plaquettaires. Ils permettent de faciliter la manipulation lors du protocole en laissant plus de temps au praticien pour injecter le PRP dans les tissus biologiques opérés.
La critique de ces techniques médicales est la nécessité d’utiliser une centrifugation à haute vitesse pour leur fabrication.
Cette technique permet d’obtenir principalement que des plaquettes sanguines, ce qui n’entrave cependant pas leur efficacité, dans la plupart des cas.
Pour autant, partant de cette carence de la technique, un autre concentré plaquettaire autologue sans apport d’antiagrégant plaquettaire a été mise au point en France par le docteur Joseph Choukroun.
LA DENTISTERIE RÉGÉNÉRATIVE EST UNE RÉVOLUTION MÉDICALE MAJEURE
Au sens commun, le terme “régénération” désigne l’ensemble des phénomènes de réparation d’un tissu ou d’un organe jusqu’à la récupération de son intégrité initial. L’organisme remplace ou restaure un tissu ou un organe du corps, lésé ou amputé, dans sa forme et sa fonction initiale.
Le terme “cicatrisation” est plus restrictif, puisqu’il désigne une modalité de la régénération au sens large : Soit, par le phénomène de régénération, une réparation d’un tissus ou d’un organe, mais pas forcément ad integrum ; soit, par le phénomène de consolidation, la réconciliation d’élément séparés qui étaient auparavant unis.
La “médecine régénérative” a comme objectif la stimulation des phénomènes de régénération afin de remplacer des tissus ou des organes endommagés ou amputés par des organes ou tissus fonctionnels au plus proche de leur intégrité initiale.
L’utilisation des « facteurs de croissance plaquettaires » et des cellules souches est un élément majeur de la médecine régénérative.
La “dentisterie régénérative” est la correspondance de la médecine régénérative au domaine de la dentisterie. Cette spécialité s’est considérablement étendues grâce aux nouvelles techniques chirurgicales de pose d’implant dentaire et de greffes osseuses et de greffes de gencive. La régénération des tissus de la cavité buccale est un sous domaine de la chirurgie orale qui est largement étudié puisque de la reconstruction des tissus osseux (tissus durs) et des tissus gingivaux et muqueux (tissus mous) dépend largement la reconstruction des arcades dentaires par des implants dentaires et des prothèses dentaires implanto-portées.
L’introduction dans le monde de la santé des concentrés sanguins plaquettaires autologues et la notion d’apport de facteurs de croissance en concentration supra physiologique est une révolution médicale majeure parce qu’elle améliore considérablement les techniques chirurgicales et les thérapeutiques médicales dans de nombreux domaines de la médecine et de la dentisterie.
En chirurgie orale régénérative : l’utilisation de PLATELET-RICH PLASMA – PRP et de PLATELET-RICH FIBRIN – PRF optimise les résultats, notamment dans les techniques chirurgicales d’implantologie : la pose d’implants dentaires et les thérapeutiques chirurgicales par des comblements osseux avec des biomatériaux, ainsi que les greffes osseuses et gingivales.
En médecine esthétique et de « réjuvénation » : l’injection de PRP ou PRF dans la peau, oblige les tissus à se régénérer pour entraîner un “rajeunissement” du visage. C’est un protocole indiqué pour repulper le visage, ou pour stimuler la repousse des cheveux s’il reste assez de bulbes capillaires au patient.
La réduction des cicatrices : elle se fonde sur le même modèle biologique de régénération.
Les douleurs articulaires : lorsque les articulations ont été prématurément usées par un travail répété ou par un traumatisme, les douleurs peuvent être tempérées ou même totalement éradiquées grâce aux injections de PRP ou de PRF qui induisent une cicatrisation tissulaire des tissus articulaires.
LA DENTISTERIE RÉGÉNÉRATIVE : L’UTILISATION DES PRP ET DES PRF
Ces deux dernières décennies ont vu le développement de nouveaux protocoles médicaux utilisant la propre biologie du patient et les capacités du corps humain à se régénérer. Ils augmentent le succès des techniques chirurgicales comme les reconstructions par des comblements osseux préimplantaires : il s’agit d’utiliser, à des fins thérapeutiques, en plus des biomatériaux, des concentrés sanguins autologues comme le PRP (Platelet-Rich Plasma ou Plasma Riche en Plaquettes) et le PRF (Platelet-Rich fibrin ou Plasma Riche en Fibrine).
Le concentré sanguin autologue s’obtient par une simple prise de sang par le praticien au cabinet dentaire. Par centrifugation du sang du patient on obtient un concentré de plaquettes sanguines contenant nombre de facteurs de croissance, dont des Bone Morphogenetic Protein (BMP2) et des Stem Cells (cellules souches).
L’utilisation de ces facteurs de croissance, des leucocytes et des cellules souches est un nouveau paradigme dans la médecine, les techniques chirurgicales et la dentisterie. C’est un temps opératoire qui stimulent la régénération des tissus, en général, et la cicatrisation osseuse, suite à l’intervention chirurgicale.
La dentisterie régénérative est un temps opératoire supplémentaire lors des techniques chirurgicales. Cette thérapeutique favorise la régénération naturelle des tissus de la cavité buccale. Elle optimise la cicatrisation osseuse et gingivale par l’apport, en quantité supra physiologiques, des facteurs de croissance biologique, inducteurs de croissance et de cicatrisation tissulaire, contenus dans le sang du patient.
Il s’agit là d’un nouveau paradigme médical : provoquer (on dit induire) la régénération des tissus biologiques lésés du patient, en se servant de ses propres cellules cicatricielles, plutôt que de les réparer à l’aide de matériaux exogènes. Les concentrés sanguins autologues prélevés sur le patient sont réinjectés immédiatement. Grâce à l’engouement que les PRP et les PRF ont entraîné, le concept de “médecine et dentisterie régénérative” est né.
Le PRP® fut la première génération de concentrés plaquettaires autologues et le PRF® est actuellement la deuxième génération.
Tous deux sont dit “autologues” car issus du sang du patient. Le premier continent un antiagrégant plaquettaire et l’autre non. Les “facteurs de croissance” qu’ils contiennent accélèrent et potentialisent la cicatrisation de la gencive et des structures osseuses blessées. C’est le principe même de la régénération tissulaire: réintroduire dans les plaies lors des techniques chirurgicales ou les tissus lésés en quantité supra-physiologiques des plaquettes sanguines et des cellules du groupe plasmatique cicatrisantes. Ces dernières comportent des facteurs moléculaires qui provoquent la régénération des tissus et donc leur cicatrisation ou leur rajeunissement.
Les médecins ont observé une accélération du développement de l’utilisation du PRP et du PRF, notamment au cours des cinq dernières années. Les PRP sont pourtant connus depuis une vingtaine d’années aux États-Unis par le biais des publications du Professeur Arun K. Garg co-découvreur de cette technique.
Bien qu’il existe une première mention des PRF dans la littérature médicale datant de 2001, ce n’est qu’au cours des années 2012 à 2014 que les universitaires se sont penchés sur les PRF. De nos jours, plus de cinq cents articles scientifiques rapportent le potentiel de régénération tissulaire induite par les PRF
En matière de chirurgie dentaire, on appelle cet apport en facteurs de croissance la chirurgie orale régénérative. Ces apports ont quelquefois pris la place des biomatériaux, dans certaines techniques chirurgicales
- A la différence du PRP, le PRF ne contient pas de sous-produits sanguins, comme des anticoagulants en particulier d’origine animal, il n’est donc pas considéré comme un médicament. Le PRF est donc une autogreffe sanguine naturelle qui ne nécessite qu’une seule centrifugation, contrairement au PRP qui en a besoin de deux.
- La fibrine du PRP est une macromolécule rigide à jonctions tétra-moléculaires ;
- La fibrine du PRF est une molécule à jonction tri-moléculaire qui lui confère une structure naturelle et physiologique, identique à celle de la cicatrice d’un tissu lésé.
Cette différence est primordiale : la fibrine du PRF délivre les facteurs de croissance sur une période plus longue que celle des PRP. Ainsi, la cicatrisation est optimisée sur plusieurs jours.
Depuis la découverte du potentiel des PRF, les chercheurs ont procédé à de nombreuses améliorations des techniques chirurgicales pour optimiser la cicatrisation tissulaire.
Le PRF est utilisé dans la chirurgie dentaire et la chirurgie orale pour susciter la régénération des tissus gingivaux et osseux. Les résultats cliniques extrêmement satisfaisants de ces thérapeutiques chirurgicales a ainsi aidé à populariser la dentisterie régénérative.
VOUS ÊTES UNIQUE !
CAS CLINIQUES DE RÉSOPTION TISSULAIRE
RÉSULTAT CLINIQUE DE LA DENTISTERIE RÉGÉNÉRATIVE
LES CELLULES SOUCHES POUR STIMULER LA CICATRISATION DES GREFFES OSSEUSES
En matière de chirurgie orale régénérative, les cellules souches ne sont pas utilisées ou très rarement. Elles sont réservées à des cas plus complexes en milieu hospitalier. De plus, une législation sévère encadre ces protocoles qui diffèrent quelque fois radicalement selon les pays. En Suisse, par exemple, certaines techniques sont permises alors qu’elles sont prohibées ailleurs, pour des raisons purement souveraines.
Les cellules souches mésenchymateuses stimulent la cicatrisation des techniques chirurgicales. Elles proviennent essentiellement de :
- La moelle osseuse,
- La graisse autologue,
- Le sang du cordon ombilical prélevé après la naissance d’un bébé.
- Le sang périphérique,
Le prélèvement de cellules souches de la moelle osseuse exige une opération chirurgicale au bloc opératoire sous anesthésie. Le médecin transplantologue se sert d’une aiguille creuse spécifique adjointe à une seringue. Il prélève des échantillons de moelle osseuse de la partie haute des os du bassin ou dans la partie haute du tibia, sous le genou. Cette opération est réalisée à plusieurs reprises pour extraire plusieurs millimètres de moelle osseuse.
Après l’intervention, le corps a besoin de quatre à six semaines pour recréer la moelle osseuse extraite.
La moelle osseuse subit un protocole de centrifugation afin de récupérer des cellules souches qui peuvent ensuite être injectées dans le greffon ou dans la zone greffée afin d’encourager l’ostéogenèse.
Le tissu graisseux comporte des cellules souches. Les chirurgiens-plasticiens utilisent cette source dans le cas de lipostructures, notamment celles du visage. En effet, l’adjonction de graisse permet à la fois une restructuration volumique du visage, mais également l’importation de cellules indifférenciées cicatricielles.
Bien qu’utilisé depuis une vingtaine d’années, ce protocole est nouveau, surtout dans le cas d’une injection chez les patients adultes. La greffe de cellules souches provenant du sang périphérique ou de la moelle osseuse du patient est plus répandue.
Les cellules souches du sang périphérique du patient sont la source la plus utilisée pour réaliser une greffe autologue de facteur sanguins. Ces cellules sont contenues dans la moelle osseuse qui va les libérer dans le sang. Dans certaines techniques hospitalières, on stimule l’hématopoïèse à l’aide d’un médicament administré au patient. Ainsi, on stimule le passage d’un nombre plus important de cellules souches hématopoïétiques de la moelle osseuse à la circulation sanguine par rapport aux taux habituels.
La technique classique consiste à faire une simple prise de sang et à concentrer les produits sanguins par centrifugation.
LES BMPS OU BONE MORPHOGENETIC PROTEINS (BMP2)
Les Bone Morphogenetic Proteins (BMPss) ou protéines morphogénétique osseuses jouent un rôle important dans la le développement de l’os et du cartilage. Ce sont des protéines appartenant à la famille des facteurs de croissance en interaction avec les cytokines ou métaboligènes inductrices. C’est à dire qu’elle entraînent la formation d’os et de cartilage. Les BMP sont désormais vus comme un ensemble prépondérant dans les signaux morphogénétiques qui orchestrent la structure tissulaire du corps humain.
Comme beaucoup d’autres protéines de la famille des BMP, les BMP-2 jouent un rôle dans les processus d’ossification, ce qui les rend intéressants dans les protocoles de greffes osseuses préimplantaires. Cependant, du fait de la rareté d’études cliniques dentaires à leur sujet, et de leur non-autorisation actuelle de mise sur le marché médical en France et en Suisse, les BMP2 ne sont pas exploités en chirurgie dentaire comme elles le sont ordinairement aux USA.
IMPORTANT: Il est à noter que tous les chapitres concernant l’usage des PRP (Plasma Riche en Plaquettes) et les cellules souches dans les protocoles de médecine régénérative sont rédigés à titre d’information générale. En effet, la législation de certain pays, comme par exemple la France, n’accepte pas encore ces protocoles novateurs. Alors que de nombreux autres pays les ont d’ores et déjà validés, comme la suisse, de même que toutes les thérapies fondées autour des cellules souches (Stem cell), en particulier aux USA. L’usage de certaine technique est pour le moment réservé au milieu hospitalier. La législation pour leur usage dans les protocoles curatifs semble être plus souple, en France comme en Suisse. C’est techniques sont de toute façon, très discutées car les avantages sont indubitables. De nombreux praticiens pionniers oeuvrent pour que les avancées de la législation soient symétriques à celles de la science et de leurs applications thérapeutiques tant curatives qu’esthétiques.