SMILE MAKEOVER
REPLACE ALL YOUR MANDIBULAR TEETH
PROTOCOL FOR IMMEDIATE LOADING OF IMPLANTS IN THE LOWER JAW
THE REHABILITATION OF YOUR DENTAL ARCADE IN THE LOWER JAIN:
THE MANDIBULAR IMPLANT PROTOCOL IN MCI



WHAT ARE THE FUNDAMENTAL SURGICAL PRINCIPLES TO BE CONSIDERED IN THE MCI PROTOCOL FOR THE MANDIBLE?
- If your clinical case allows for an implant extraction with immediate loading, there are three basic operative points to consider:
- Firstly: The diseased teeth must be extracted at the time of implant placement: This so-called extraction-implant technique minimizes the physiological and unavoidable post-extraction alveolar bone resorption.
Indeed, the decisive point of our protocol is to place the implants innative bone (the patient’s original, non-grafted bone) at the time of tooth extraction to preserve sufficient height and width of the bone wall (alveolar bone where the teeth are located) necessary for implant placement.
It is important to understand that the alveolar bone immediately begins its physiological resorption at the time of tooth extraction.
- The apposition bone grafts must be done in the same operating time: This technique of allogeneic and/or xenogeneic bone grafts is done from banked bone, either allogeneic (human origin) or xenogeneic (animal origin, generally ovine).
- Enrichment with autologous platelet tissue growth factors: Bone grafts are systematically enriched with aPRF in membrane form and iPRF in liquid form. See the chapter “Booster stem cells PRF” on “regenerative dentistry”.
The principle of the protocol for placing implants in immediate loading is to perform exactly the same surgical procedure as in the upper jaw.
Consequently, the costs are almost identical unless special pre-implant bone grafting procedures are to be considered. The anatomy of the lower jaw, also called the mandible, has nothing to do with that of the upper jaw. The limiting anatomical elements are less important in the lower jaw than in the upper jaw. The problem of the proximity of the pneumatized maxillary sinuses makes the interventions very complicated in the upper jaw.
In the mandible, the limiting factor is essentially the bone resorption of the horizontal branch of the mandible. That is, the posterior part behind the canine teeth.
The most limiting anatomical obstacle is the alveolar dental nerve, which runs beneath the molars and premolars. It emerges from the mandibular bone just below the roots of the premolars.
When this area of bone is heavily resorbed, there is too little height between the top of the alveolar bone ridge and the inferior alveolar nerve to place implants.
Fortunately, the new concept of mini implants, i.e. implants with a height of 6 to 8 mm, now makes it possible to place implants despite a very low available bone height.
If, however, the height was totally insufficient, certain pre-implant surgery techniques make it possible :
- Either graft the resorbed area with bone bank enriched with cellular growth factors contained in platelet concentrates and a matrix system (like a mold). The purpose of this procedure is to raise the bone level above the mandibular alveolar ridge. However, these surgical protocols are very recent and have little experience. In particular, we do not know what will happen to this grafted bone with time? Et whether it will be reduced or not? even if implants are placed there.
- There is also a surgical protocol to reroute the inferior alveolar nerve to place it outside the bone in the cheek. Exactly as it happens for most of the nerve bundles of the face. This is not a problem for the sensitivity of the lip and chin. However, there may be accidents and injury or rupture of this nerve. The paresthesia after-effects are normally temporary but can be permanent in the case of serious surgical hazards. The objective of these rather risky procedures is to free up the vertical space of the horizontal branch of the mandible so that implants can be placed there.
- The risk-free solution is the use of modern supra-implant prosthetic systems: once a sufficient number of implants have been placed, premolar and molar extensions at the ends of the implant-supported bridge of at least 12 mm in length (one molar) can be made. Therefore, it is possible to extend the prosthetic arch at the level of the premolars and molars with these extensions without the need to place implants in the posterior areas.
WHAT ARE THE THREE MAIN TECHNICAL DIFFICULTIES TO OVERCOME IN ORDER TO SCREW IN AN IMPLANT-SUPPORTED FULL BRIDGE IN IMMEDIATE LOADING ON THE LOWER ARCH?
The first difficulty is the degree of initial vertical and horizontal resorption of the lingual wall (behind the lower teeth) in the anterior region where the implants are to be placed.
The guiding principle of our surgical techniques is that the alveolar bone wall must be sufficient and stable over time, in all 3 dimensions of its volume, to place implants.
To respect this principle, it is necessary to use operating techniques:
- Which avoid losing the necessary alveolar bone height to make a prosthesis with the right vertical dimension of occlusion (DVO);
- Which block bone resorption to the maximum by inducing bone regeneration: regenerative dentistry;
- Anticipate bone loss or correct the one already present, by rebuilding bone volume in an optimal way: bone grafts + Rich Fibrin Plasma
Consequently, as we have already seen, the teeth should preferably be extracted at the time of the implant placement procedure in order to block any disastrous bone resorption.
If, on the other hand, the dental extractions were done a long time ago, then the jawbone has already been greatly resorbed.
Or, if the periodontal disease (loosening of the teeth) is old and almost terminal, then the alveolar bone along the roots has already been destroyed over a very large height.
In these cases, the aesthetic result with the satisfying impression that the ceramic dental crowns screwed onto the implants are literally “sticking out” of the gums will be very difficult to achieve.
The solution is to make a false gum (preferably with a pink ceramic cosmetic) applied around the ceramic teeth of the implant-supported bridge.
Unfortunately, this is sometimes an aesthetic necessity, to compensate for mandibular bone loss while preserving the harmonious natural height of the dental crowns of the implant-supported bridge with ceramic (or composite) cosmetics: it’s an epithesis that replaces the missing part of the mandibular alveolar bone, included in the cosmetics of the implant-supported dental bridge.
The height of the teeth and the vertical occlusal dimension (VOD) is determined by the degree of vertical resorption of the lingual wall in the anterior region where the implants are to be placed.
- The correct vertical dimension of the lower face (DVO): it is determined by the height of the teeth.
- In order to maintain or regain this vertical dimension of the lower face (DVO) without a “long teeth” effect, we will sometimes be obliged to fabricate a ceramic false gum around the ceramic crown between it and the intraosseous dental implant. In this way, we can raise the implant-supported bridge, without having an effect of abnormally elongated teeth, which is very unsightly.
This ceramic (or composite) false gingiva is totally invisible to those looking at you.

The second difficulty is a loss of the normal anatomy of the upper dental arch due to very decayed teeth and therefore a destructured inter-maxillary occlusion.
However, to make this type of very sophisticated MCI prosthesis, it is imperative to have an ideal occlusion between the two arches (upper and lower).
This will require:
- Or perform reconstruction work on the antagonist arch with a series of treatments on your natural teeth and defined in another treatment plan;
- Or seriously optimize the prosthetic solution you currently have with another temporary prosthesis.
These various interventions to resolve these difficulties will be performed in parallel with the placement of implants on this mandibular arch.
- Or perform an MCI procedure on both arches in the same operative time frame.
The third difficulty is the passage of the inferior alveolar nerve (NAI) which runs in the horizontal branch of the mandible under the lower molars and premolars:
The inferior alveolar nerve (NAI) is closer to the bone surface (in the posterior and inferior area) the more your mandibular bone is resorbed from past extractions.
What are the difficulties:
- If the dental nerve is within 8 to 6 millimeters of the top of the usable bone ridge, then implant placement is almost impossible in this state.
Additional grafts to increase this height can be considered.
- The risk is an injury to the lower dental nerve at the time of implant placement that could generate paresthesia of the lip and chin on the side of the procedure.
What are the solutions:
- However, it is generally possible to place between 6 and 8 implants in the mandible, with 2 short or mini implants of 4 to 8 mm in height, in the two posterior areas (right and left).
- But only if the dental nerve is within a few millimeters (between 10 and 8 millimeters) of the usable bone surface of the alveolar ridge.
Below this minimum height a strategic decision must be made:
- Or perform a vertical bone augmentation graft;
- Either perform an inferior alveolar nerve (NAI) diversion;
- Or opt for an implantation only on the anterior part of the mandible, with a possible prosthetic extension to the posterior ends.

OVERVIEW OF SURGICAL SOLUTIONS PERFORMED AT THE TIME OF IMPLANT PLACEMENT TO OVERCOME DIFFICULTIES SPECIFIC TO THE ANATOMY OF THE LOWER JAW
Systematization of allogeneic and/or xenogeneic appositional bone grafts associated with PRF to compensate for bone resorptions:
Bone grafting is performed around the entire circumference of the implanted arch. The purpose of this procedure is not only to fill the bone gaps resulting from tooth extractions, but also to compensate for the physiological resorption of the mandibular alveolar bone.
It will be systematically done, at the time of implant placement, to compensate for the inevitable post-extraction physiological bone resorption and possible bone gaps.
This large bone graft, covering the entire circumference of the mandibular bone, helps to regenerate this piece of bone and, in a way, compensate not only for the effects of age that have already occurred, but also to anticipate future physiological bone resorption.
IS IT POSSIBLE TO FIT A MANDIBULAR IMPLANT-SUPPORTED BRIDGE IN MCI ALL ON 6 OR ALL ON 8
IN WHICH CLINICAL SITUATION?
If the vertical and horizontal bone resorption of the anterior AND posterior bone walls is not too great, or is compensated for by bone grafts, then the bone volume is sufficient for implant placement.
In this case, the placement of implants in the posterior sectors is just as feasible as in the anterior sector.
In this configuration, it will be possible to make a molar-to-molar screw-retained implant-supported bridge with 6 to 8 implants.
This is the All on 6 or All on 8 technique, depending on whether six or eight implants are placed in the mandible.
The number of implants depends of course on the available bone volume but also on the size of the patient.
- This option is ideal because it fully restores the masticatory function and aesthetics of the smile.
- Most of the time, even if the posterior areas are resorbed, it is possible to place mini implants above the inferior alveolar nerve without damaging it.
- If bone resorption has led to almost total atrophy of the posterior part of the horizontal branch of the mandible and it is not possible to place implants in these posterior sectors. However, there are several solutions to remedy this problem: it is possible to reroute the inferior alveolar nerve, by taking it out of the jaw, or to perform a bone graft to increase the vertical volume. However, the most common solution consists of making extensions at the posterior ends of the bridge that replace either the premolars in the worst case, or the molars in the best case.

THE RESILIENT BRIDGE FOR IMMEDIATE LOADING WILL BE SCREWED ONTO THE IMPLANTS A FEW DAYS AFTER THE IMPLANT SURGERY
We call this resilient bridge screw-retained on the implants: The “resilient bridge for immediate loading of implants”.
(Resilient Implant-supported Full Arch Bridge with Immediate Loading – RIFA Bridge with IL)
Why is the immediate implant loading bridge called “resilient”?

The resilient bridge for immediate loading of implants : she metallic skeletal structure or framework or central beam:
It is designed and manufactured with the help of the computer (a 3D laser printer for metal CAD/CAM) in a metal alloy (titanium or chrome cobalt). Its manufacturing precision is exceptional. This performance in micro-mechanics allows a total mechanical passivity when this framework is screwed on the implants.
The metal alloys used are sufficiently ductile (can be stretched without breaking) to absorb the shocks and pressure of chewing and swallowing.
At the same time, it is sufficiently rigid, without breaking, so that once screwed onto the implants, it guarantees their immobility with a tolerance of movement of less than 200 microns, in order to avoid micro-movements that are fatal to osseointegration (healing of the bone on the implants).
The resilient bridge for immediate implant loading The composite or hybrid cosmetic material.
The hybrid material of the composite family is a highly resilient biomaterial resin that absorbs the shocks of chewing and swallowing thanks to its flexibility.
Moreover, thanks to its physical aesthetic properties, it reproduces a quasi mimicry of natural teeth, in particular the teeth of the smile.
It is also made with 3D CAD/CAM technologies which allows a perfect reproduction of the dental anatomy.
The composite provides resilience to the whole, absorbing the energy of chewing shocks to protect healing implants:
- This resilient bridge screwed onto the implants solves the dilemma of an immediate loading that must be both very rigid and “soft”.
- This resilient bridge protects the implants from micromovements of more than 200 microns and from shocks that cause disosteointegration and healing failure.
- At the same time, this resilient bridge is aesthetically pleasing thanks to the aesthetic qualities of the hybrid material.
The resilient bridge will be screwed in between 2 and 7 days postoperatively: this is the time it takes for the prosthetic laboratory to create a very high quality custom-made bridge that can be considered as final.
- This resilient bridge will be left in place for a minimum of 6 to 12 months for healing and maturation of the hard tissue (maxillary alveolar bone) and also soft tissue (gingiva and oral mucosa).
- This resilient bridge is different from a traditional “temporary” or “transitional” resin bridge. Its skeletal structure is manufactured in exactly the same way as a permanent ceramic bridge. This is not the case with the skeletal structures of traditional “temporary bridges” made of resin or even reinforced with a metal arch (sometimes welded intraoperatively). This mechanical quality allows for prolonged use.
- This resilient bridge differs from a “provisional” or “transitional” bridge made before implant placement, following surgical planning using “All on 4” or “All on 6” implant simulation software. The localization impression of the newly placed implants is made extemporaneously during the operation. It allows us to make an exact replica of the dental arch and the smile ideally imagined after the implant surgery.
Our MCI implant placement protocol is different from an implant “surgical planning”: because our implantologists want to have a permanent control on their surgery, thanks to a total possibility of adaptation and flexibility per and post operative.
A protocol with a preoperative planning and/or implant navigation technique is, by nature, more fixed and more difficult to modify during the operation according to surgical hazards. It is often said that one “does not operate a scanner” and adjustments during the operation are very frequent.

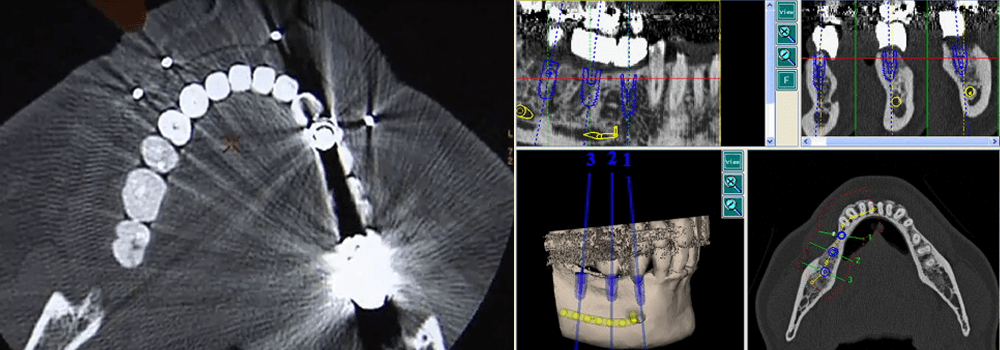
Preoperative implant planning techniques or intraoperative implant navigation
At Smile Designer, our implantologists currently prefer the immediate loading implant protocol described in these pages, but we are no strangers to pre-operative implant planning protocols.
In the following link you will find a series of films, made at the time, dedicated to a digitalized surgical navigation system for pre- and per-implant surgery.
It is a computerized robotic system that allows, following the acquisition of a scanner and a computerized planning of the placement of implants, to perform this intervention with a digitalized surgical guide. A radar guides the surgeon’s hand on the computer screen. This allows us to verify that the position and axis of the implants are in accordance with the pre-operative planning. Even if this tool is quite interesting (especially for the time because it is an old technique) the habit and the experience of many protocols led our surgeons to conclude to prefer the method that we describe.
Of course, this opinion is only binding on our practice. Some talented colleagues are much more comfortable with this type of assistance.
However, even if we do not use intraoperative guidance tools such as physical or digital implant guides, all our procedures are duly planned on a computer using implant planning software:
The main criticism that we have of physical or digital implant guides is that they are difficult to adapt immediately intraoperatively to all the hazards that cannot be identified on the scanner. This immediate and instinctive “adaptation” during a surgery is in the nature of the surgeon. But it is technically dependent on the experience and training of the operator.
Because as the saying goes in the implantology world: “you can’t operate on a scanner”! Even though this examination is totally indispensable.
digital surgical navigation with the ROBODENT system
preoperative planning and implant navigation techniques
AFTER THE HEALING PHASE OF THE IMPLANTS WE GIVE YOU TIME TO REPLACE THE RESILIENT MCI BRIDGE WITH A FINAL IMPLANT-SUPPORTED CERAMIC BRIDGE
Our professional philosophy obliges us to conceive our profession in the most deontological and ethical way possible: this is why we try to give access to our protocol to as many of you as possible.
By deciding to do this rehabilitation of your mouth and your smile, you have started a new slice of life. This intervention is important from all points of view. We are all aware that it will determine a “before” and an “after”. The burden is multiple, both physical, emotional and financial. It is frequent that patients are in a situation of dental distress but also financial. In this situation, the patient needs to be rapidly reconstructed with an implant-supported composite bridge in immediate loading. But he may not be able to bear the financial burden of a permanent bridge with a ceramic cosmetic within a few months.
Thanks to our MCI protocol, we are able to both compact the treatments to give you back your smile in an extremely short period of time and also to provide you with long-term care.
We are also perfectly aware that we are the bearers of hope for a large part of the population who are in a situation that is either already dramatic or on the verge of collapse with teeth that, if they deteriorate even more or if they are not restored quickly, will tip people into premature aging and a handicap in terms of chewing comfort, healthy food and taste and, of course, in terms of professional and emotional social relationships.
However, the costs of this type of intervention are limiting for a large part of the population. We have therefore thought of solutions to give the greatest number of people access to our protocol and not to shatter the hopes of a part of the public waiting for medical solutions to this type of problem.
Once again we are faced with a dilemma!
That is to say, how to choose between two contradictory proposals, both unsatisfactory. How to solve the dilemma of affordability of an extremely sophisticated and expensive protocol without reducing its quality?
There is no other alternative than to place a bridge on the implants that is of very high quality. Since we use extremely sophisticated techniques, they are naturally expensive. The training of a surgeon to master all the technical aspects of this multidisciplinary protocol is also very long and costly.
We solved this dilemma by dividing our MCI implant protocol into two major steps:
– Firstly, an implant-supported resilient bridge with composite cosmetics is used as the first-line treatment;
– Secondly, a bridge with a ceramic veneer can be placed as a second option.
We give you time to choose to optimize your smile with increasingly sophisticated techniques both aesthetically and functionally, such as the permanent ceramic bridge
- The reference option is to replace the implant-supported resilient bridge with its copy with a ceramic cosmetic after eight to twelve months of tissue maturation. This permanent ceramic bridge is more aesthetic, more biocompatible and more durable over time
- An alternative option, in the event of difficulties or personal choice, is to keep the implant-supported resilient bridge with its hybrid material cosmetics for several months or even years. Since the materials used to manufacture the implant-supported resilient bridge are of good quality, this option is theoretically possible. This theory will have to be confronted with the clinical requirements and the problems or hazards that may have occurred during the healing process. This resilient bridge can eventually be renovated, if necessary.
Thanks to new CAD/CAM technologies and new materials such as composite, our laboratory can produce a resilient bridge of the highest mechanical and aesthetic standard in just a few days.
This implant-supported bridge with composite cosmetics must be worn for several months while the implants heal.
After five to six months the implants are osseointegrated into the jawbone. It can be unscrewed and taken to the dental laboratory to be modified and corrected according to the patient’s occlusal parameters and also aesthetically improved.
Of course, it can also be renovated and repaired much more easily than a ceramic version, if the patient so desires. In general, this type of bridge is kept unchanged beyond the time required for healing, essentially for economic reasons .
The final version of the bridge in the MCI protocol, with a ceramic cosmetic, is the outcome of our protocol.
Maturation of the soft and hard tissues around the first resilient bridge is completed in about ten months. This is why the second ceramic implant-supported bridge allows for the correction of possible bone resorption due to the maturation of the soft and hard tissues for an even more refined AESTHETICS and MASTICATION.
After this period of 6 to 12 months, the implants are osseointegrated. It is no longer mandatory to load implants with a “resilient” screw-retained bridge. The implants can absorb the energy of hard shocks, generated by biting and chewing on ceramic which is a non-resilient and non-ductile material.
At this stage of the loading protocol, it is possible to replace the resilient screw-retained bridge with another ceramic screw-retained bridge that is much more sophisticated and demanding in terms of bite and esthetics.
Cosmetic ceramic material cannot be placed on implants in the first instance because it is much too hard and traumatic for newly placed implants. It risks to disosteointegrate the implants.
This second implant-supported and screw-retained ceramic bridge is fabricated with the same type of CAD/CAM metal framework. But, it has a stratified ceramic cosmetic that is even more aesthetic and more cutting and grinding for a better chewing.
We call this second intention ceramic bridge screw-retained on the implants: The “ceramic bridge for definitive loading of implants”.
(CIFA Bridge in IL: Ceramic implant-supported Full Arch Bridge in Immediate Loading)
Laminated ceramics perfectly mimic the aesthetics of the smile, as their visual qualities are even closer to those of the teeth than hybrid material.
In addition, the hardness of the ceramic allows for a much more efficient bite and chewing, especially for fibrous foods such as meat.